Talent, Friction, Engagement - Call to Tech
We have heard about the Great Resignation that happened during the pandemic. Especially in healthcare, where nursing staff exited work due to retirement, burnout, exposure risks and the stress of supply shortages.
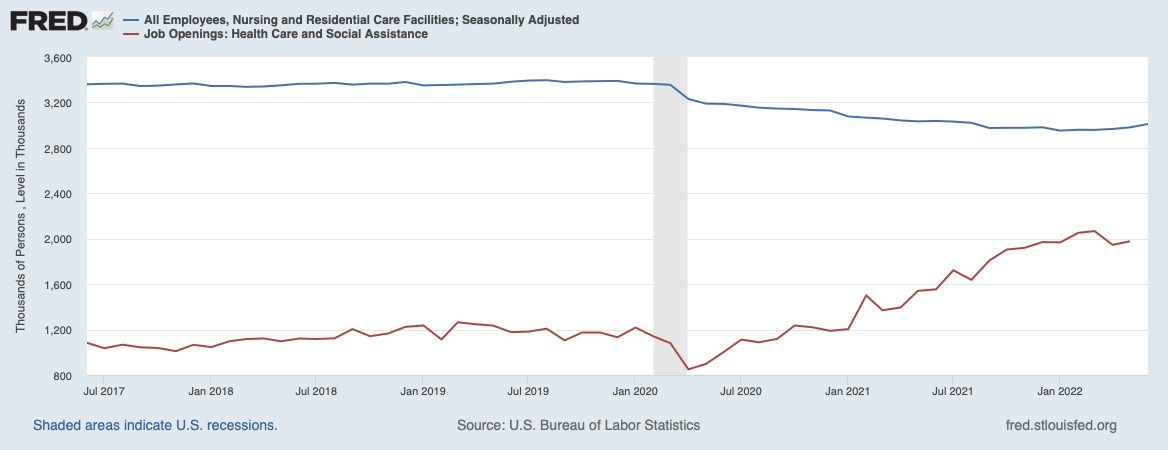
Nursing employment has begun a mild uptick since the start of this year, but the available jobs is growing faster than before, which is essentially an indicator of stretched teams and finances.
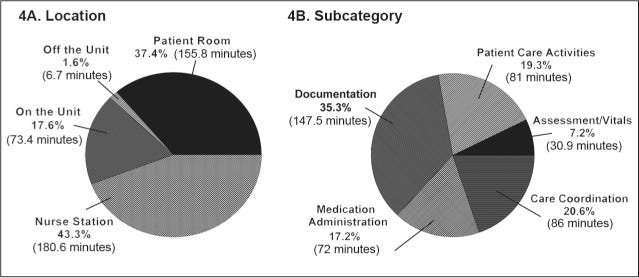
Second, consider what % of time nursing/clinical staff spend on actual care activities vs admin/less value adding work.
60+% of nurse’s time is spent outside patient room and this can be highly optimised and automated (care coordination, documentation and med admin work can be analysed and reduced through automation, better physical and information design).
This is the friction in just one part that we see everyday in health systems. Legacy tech, poor workflows (to be fair, these were designed long back and still in use in many settings) and complex apps makes it the responsibility of clinicians to navigate apps rather than apps becoming frictionless and efficient.
This has massive implications for care productivity, outcomes and adds more pressure to leaders to figure out smarter solutions. Usually, at this time, in other industries, technology (not just IT) innovation happens and balance is restored to the universe. In healthcare, this script is playing slower than expected, primarily because some enabling factors are yet to be in place fully.
What’s missing in current hospital landscape that’s preventing tech from making an impact?
There are structural reasons explained partly through Baumol’s cost disease, historical choices for Medicare/Medicaid etc. Leaving those aside, I believe a few issues need to be fixed:
Single view of patient (from traditional provider and new health firms)
Work with existing legacy to integrate work and data flows
Automate and eliminate operational friction rather than focus on clinical impact mostly.
The goal obviously is to be with Rainbows & Unicorns, where the solution delivers both on outcomes and productivity. Leaning in either direction is not a terrible strategy either: the single view of patient is critical for what I’m calling full stack condition management (CKD/ESRD - Somatus is one, Flatiron is another).
The second, ability to work with existing legacy and make the sum better than before is still not fully in focus. We see good progress in AI domain (BayesianHealth is an example), but there is lot more possible in nuts and bolts stuff like scheduling, prior auths etc which is not happening. The reason I believe is that digital health startups and traditional providers are not listening to each other.
The environment is noisy, signing the first deal with providers is not easy and its faster to get started by doing scheduling for a digital health startup rather than solve the thorny issues in a provider estate.
The third is where I’m most excited about. There is incredible amount of waste in the system, we all know that. Majority of it is due to isolated information, sullen systems and terrible risk/trust equations. Using tech on existing estate smartly to begin breaking these barriers, increase visibility and improve signal quality will be an obvious winner.
Startups that have such an overarching view are too few. We have seen a few in data sharing (Ribbon, Innovaccer etc), but there is some much that’s open: revenue cycle, cross-system billing, admin/checkin process automation are some that come to my mind immediately.
Pandemic is now a call to Health+Tech folks who are willing and capable in working with hospitals to begin solving these meaningful problems.